Infection and Global Health Research Division
Research at the University of St Andrews School of Medicine
SLIC
Scattered Light Integrated Collector
PI: Dr Robert Hammond, School of Medicine
“You can plan research … you cannot plan discovery.”
Lord Rutherford
What is the problem?
Antimicrobial resistance (AMR) is a global and growing problem. Inappropriate use of antibiotics is driving resistance in microbes meaning infections will become harder to treat in the future. This can and will change the way we live our lives. The worst-case scenario is one of society returning to a pre-antibiotic age where the discoveries of Alexander Fleming and many others count for nothing. Elective surgeries will become a thing of the past, HIV infection will once again become a death sentence and treatments like chemotherapy for cancer will become nearly impossible.
This bleak view can be reversed with careful management. Antibiotic stewardship is a policy whereby we are trying to reduce the use of antibiotic uptake in the population, only prescribing them where they are really necessary. Stewardship will mean understanding which infections can be cured with targeted therapy rather than using broad spectrum antibiotics as a ‘scatter gun’ approach.
Novel technologies that deliver useful information in a short time have been cited multiple times as a potential mechanism towards effective antibiotic stewardship.
At the University of St Andrews we have developed just such a novel technology: SLIC. The Scattered Light Integrated Collector is a step change in the way in which antimicrobial susceptibility testing (AST) is done. Due to SLIC’s exquisite sensitivity, it can detect tiny changes in microbial population. Where current photonic technology has a limit of detection (LoD) around 10,000 microbial cells in 1 millilitre of liquid SLIC’s LoD is 25 cells/mL. This translates to rapid detection of population change, either growth or decline.
Story of SLIC
SLIC began as a PhD project that set out to define the differences between the bacteria that cause tuberculosis and leprosy- Mycobacteria. These bacteria can appear short and fat or long and thin under a microscope depending on if they are stressed or not. The original SLIC (version 1) was made of soft modelling foam and a modulated laser pointer. It showed, however, that it was possible to use the baseline technology developed to do something unexpected- measure bacterial number.
SLIC Version 1
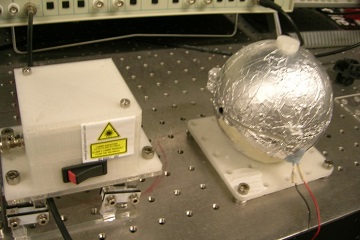
To expand upon this version 2 was made with more robust materials. It was 3D printed and surrounded in aluminium foil to stop the escape of reflected and refracted laser light. A higher power laser was mounted on a movable gimble and circuitry was used to stop power decline over the power source lifetime.
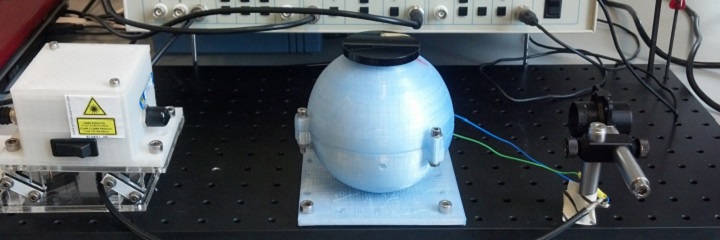
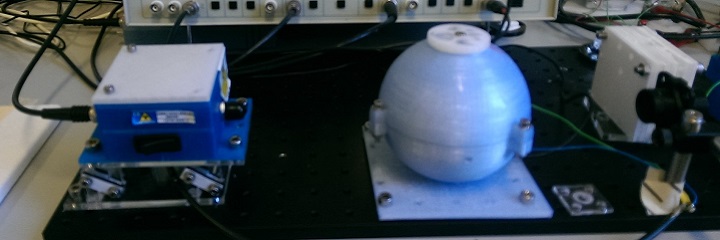
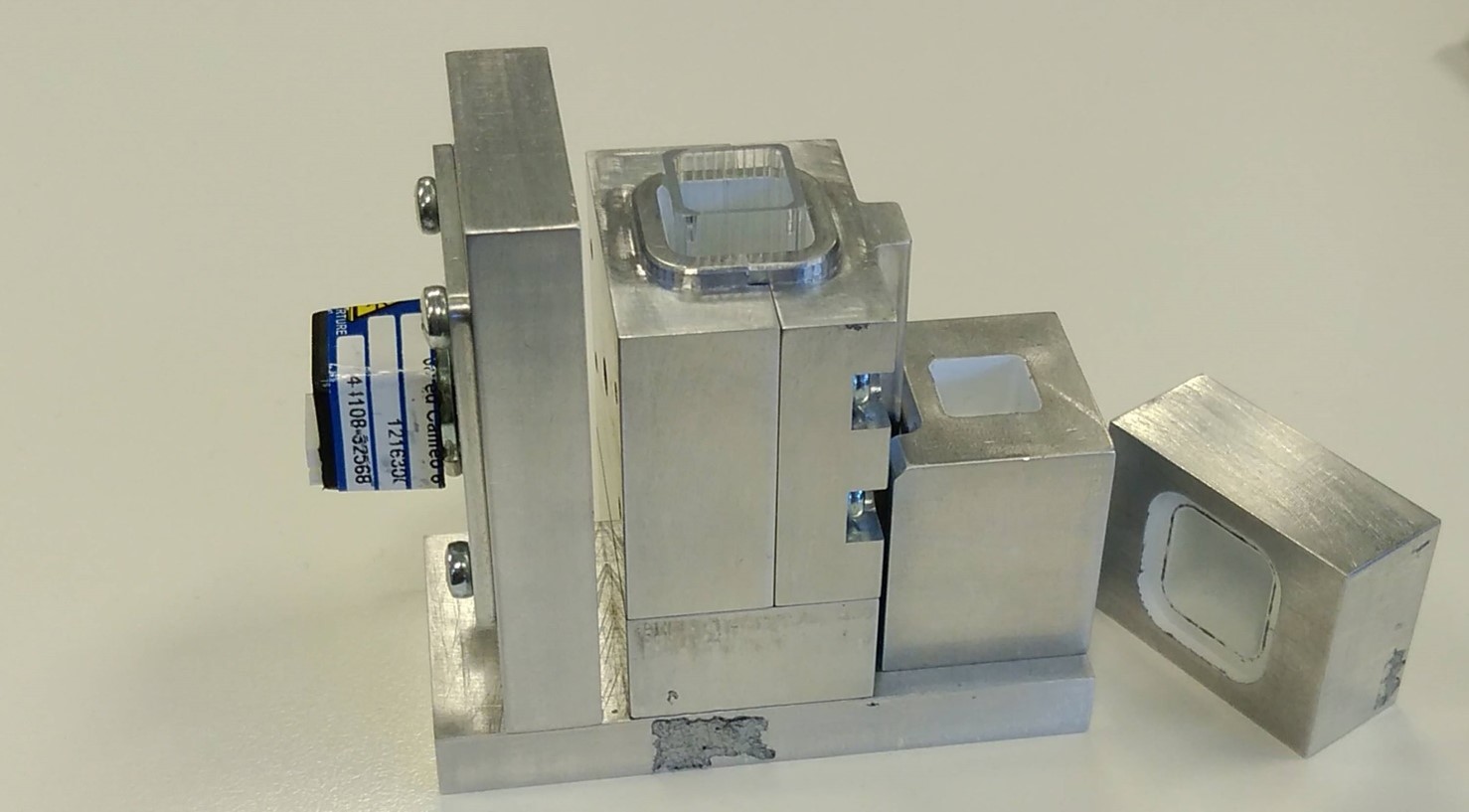
Version 3.1 was upgraded again to include a new removable sample holder and mobile beam dump for added safety. This version has light conductive internal architecture that turned out to reduce the signal rather than enhance it so version 3.2 was produced with the architecture removed and an improved power source for the laser. Other improvements included an enhanced detection array and laser misalignment sensors.
SLIC Version 3.1
SLIC Version 3.2
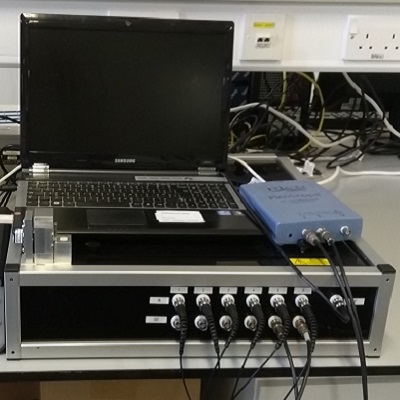
In order to further our efforts in real-time bacterial growth analysis version 4 was produced by a subsidiary company of the University. This version was interlocked to further improve safety and featured two distinct units- a bench top processing unit and an in-incubator laser and detection unit. With version 4 we collected our first real-time data and thus proved that the SLIC technology was applicable to real clinical scenarios.
To move beyond single sample testing we commissioned an outside contractor to produce the next version of SLIC. As a proof of principle version 5 was produced with entirely new geometry, photodetection and multiplexing possibilities.
Due to the success of version 5 a full-scale version 6 was produced that allowed multiplexing of 6 samples simultaneously. For the first time we could run a full antimicrobial panel and collect real-time data with real clinical impact. This version still consisted of 2 sub-units, a benchtop and an incubator unit. The final stage was to combine this and make the device self-incubating.
Versions 6.1, 7.1 & 8 are self-incubating fully self-contained units that have been shipped all over the world. These robust machines multiplex 6-16 channels, report data in real time and have been shown to correlate with the state of the art technologies in hospitals in terms of accuracy (>98% agreement) but supersede them in terms of sensitivity, precision and rapidity. They can be used in place of current technology, testing microbes from patient derived pure culture but they can also be used to directly test fluids and swabs from patients.
SLIC around the world
SLIC machines are being used throuout the University of St Andrews for a variety of microbiological tasks. We are researching the effects of novel antimicrobial agents with colleagues from chemistry, developing new drug-free treatment options with colleagues from physics, using SLIC with dangerous pathogens in our category 3 biohazard containment facility and developing enhanced software to analyse the data generated by these exciting projects.
Additionally SLICshave been shipped to and used in various locations around Scotland and the wider UK- Ninewells and King Cross hospitals in Dundee, Dundee University, and to various GP practises around Fife to run limited clinical trials. Machines also exist with collaborators in Cambridge, London universities and the Royal Preston hospital, Lancashire.
We have collaborations in Łódź, Poland and are aiming to collaborate with other European sites. We also have an active collaboration with Kenya where SLIC machines will be used to test patient urine for resistant organisms and a new partnership with Ecuador do conduct similar research.
How we are solving the problem?
In 2014 the NESTA Longitude prize was launched. This is a £10m prize the subject of which was voted for by the public. The public vote decided that AMR was the single largest crisis facing the world and that a 30 minute AST test was what was required. Thus, teams, institutions and companies around the world began creating tests to meet this challenge. SLIC has risen to this challenge and in 2016 was awarded a Longitude Prize Discovery Award, recognising SLIC’s potential to avert an AMR crisis. In 2018 SLIC was further recognised by the Scottish Life Sciences Institute and we received the Innovation of the Year Award.
The capacity to detect antimicrobial resistance in real time and in under 30 minutes changes the face of microbiological health care. Where previously a result might be returned in 24-48 hours now the technology exists to have a comprehensive result returned to the patient and attendant clinician in under 1 hour. This will have ramifications for patients in both high and low-risk groups where a rapid result can be the difference between life and death.